- NHIF rural beneficiaries face charges for essential services amid a funding dispute with RUPHA
- RUPHA cites a six-month delay, impacting outpatient, surgery, and cancer care services
- Emergency and Critical Situations remain unaffected; RUPHA urges government fund disbursement
Beneficiaries of the National Hospital Insurance Fund (NHIF) in rural areas are now required to bear the cost of vital health services. This decision stems from the Rural Private Hospitals

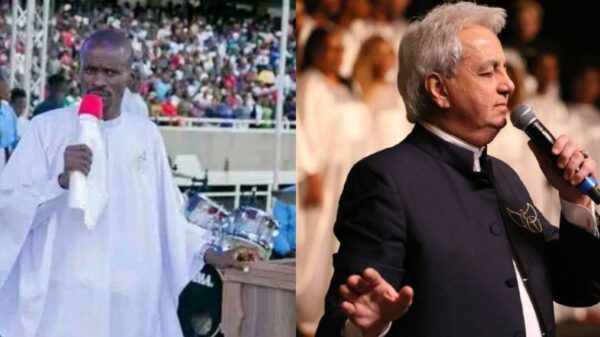
NHIF headquarters
Photo: Courtesy
Association of Kenya (RUPHA) following through on its threat to suspend certain medical services covered by NHIF due to the government’s failure to disburse funds for the past six months.
RUPHA, in a statement, highlighted a deadlock with the government, leading to the association’s decision. Notably, outpatient services now demand a payment of Ksh.1000 for treatment. Surgery will incur theater fees, and cancer care will require beneficiaries to cover consultation fees, laboratory testing fees, and procedure fees.
Even beneficiaries of the Linda Mama Scheme are not exempt, as they will now be asked to pay a procedure fee for normal delivery and a theater fee for a Caesarean section. RUPHA clarified that the Emergency and Critical Situations section will remain unaffected, ensuring continuous patient care without alterations.
The association, expressing regret for the impact on the public, reiterated its plea to the government to promptly disburse funds for seamless service delivery. RUPHA Chairman Dr. Brian Lishenga, in a letter to NHIF Board Chair Eng. Michael Kamau, issued a seven-day notice last month, emphasizing that the delay in fund disbursement violates the law.
“It has come to our attention that as of 8th December 2023 and for the last 6 months, the Board has failed to make the required payments to health facilities in strict compliance with the provisions of our Agreement,” stated Dr. Lishenga.
“This non-payment of healthcare providers represents a persistent and clear breach of our agreement with NHIF.”